FAQs and Getting to My Diagnosis
FAQs
For our family and friends to whom we haven’t been able to communicate these details directly, I wanted to include some more information here on our situation and help provide clarity.
What’s my diagnosis?
Classical Hodgkin’s Lymphoma Stage 2a. The cancer cells are located in my neck and chest. I’m considered “early favorable” because of my staging and because I do not have additional risk factors that would increase the chance of the cancer returning after it is treated.
My diagnosis is excellent news as this type of cancer has around a 90% cure rate. We are so grateful and have every reason to hope that I’ll respond well to treatment.
What is Hodgkin’s Lymphoma?
Hodgkin’s Lymphoma is a type of blood cancer that develops in the lymphatic system. It starts when an abnormal change to the DNA of a white blood cell (called a lymphocyte) causes it to become a lymphoma cell that results in the uncontrolled growth of cancerous lymphocytes.
These cancerous cells crowd out normal white blood cells, and the immune system can't guard against infection effectively. It occurs most frequently in two separate age groups: first in young adulthood (ages 15–35) and the second in those over 55 years old. The annual number of cases is 2.7 per 100,000 persons per year, and it accounts for slightly less than 1% of all cancers.
What are my symptoms?
I had swelling on the side of my neck and multiple enlarged lymph nodes starting in January. I’ve also had persistent fatigue for many months, but I just attributed this to…you know, life! I was sick a lot over the last year with several colds/flus, multiple new skin conditions, and bouts of food poisoning. The fatigue and more frequent illnesses now make sense in light of my diagnosis and seem to indicate my immune system has been suboptimal for some time.
What’s my treatment plan?
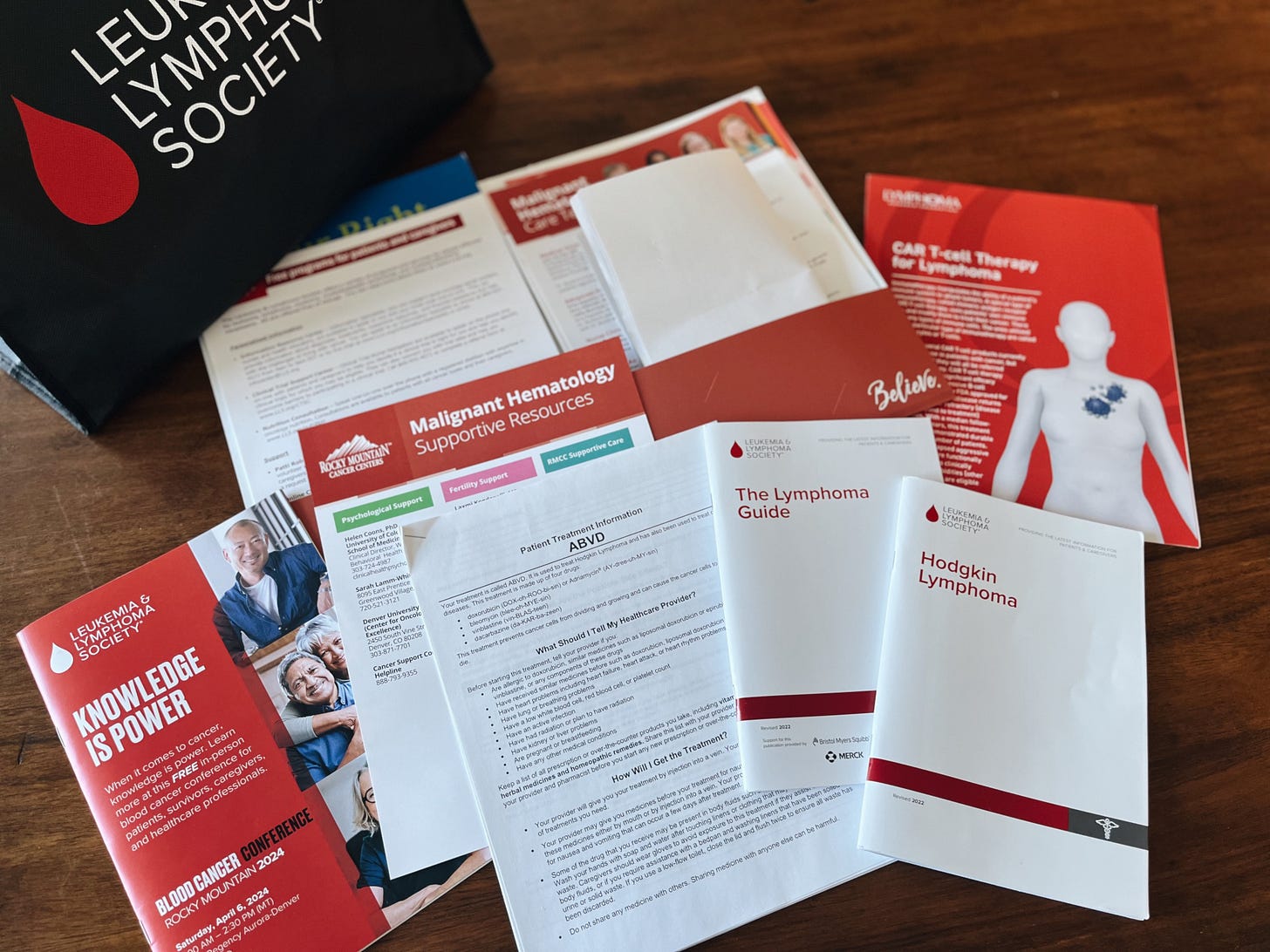
Treatment for Hodgkin’s Lymphoma includes chemotherapy and/or radiation. My chemotherapy regimen is called ABVD, which is currently the standard treatment for this disease in the US. The abbreviation stands for the four drugs adriamycin, bleomycin, vinblastine, and dacarbazine.
I will receive 8 chemo infusions over the next four months, spaced out every two weeks on Thursdays or Fridays. My first chemo infusion was originally scheduled for April 19 — this is currently pending (see 4/17 update here). Right now, my plan is to take 1-2 days off of work for each chemo infusion and try to rest and recover over the weekends.
I’ll have a PET scan halfway through to check that I’m in remission and those results will inform the latter half of treatment.
Possible radiation is something we’ll have to consider toward the end of treatment and discuss trade-offs. Data currently shows that patients can benefit from about an extra 7% increase in avoiding recurrence if they receive radiation, but given that they would need to target my neck and chest, it may also predispose me to breast and thyroid cancers, and lung and heart damage. Our early inclination is to forgo radiation given these risks.
Getting to my diagnosis
Below is a summary of the steps we took up until now to get to my diagnosis. Overall, I’m thankful that we were able to move relatively quickly. It took roughly two months from the onset of my first symptom to get my preliminary diagnosis, and one more month from that to begin treatment.
Coordinating and attending these medical appointments has felt like a part-time job with how much time and energy they require. It has also been a huge investment of time and emotional energy to research and process information, stay on top of medical and job communications, share our initial news and then subsequent updates to family and friends near and far, and prepare for the start of treatment. It wasn’t something I’ve experienced before and it’s increased my empathy for anyone who’s caught up in something similar. Thank God for grace — how deeply we all need it when life gets chaotic!
January 18: I woke up with lots of neck pain but didn’t think too much of it. We had been in Alabama for the last week visiting friends and family. Back home in Denver, it had dropped into the single digits during the first big storm this winter and a water pipe had burst in our apartment. It took a couple of days to complete repairs and restore heat so for the next two nights we embraced at-home glamping and slept in our sleeping bags. The temperature had dropped so low that our memory foam bed and pillows had become cold and stiff so I attributed my poor sleep and sore neck to that.
January 20: Thankful to have our home heated back up, I woke up this morning with significant swelling on the right side of my neck.
January 25: My first appointment was with my PCP. My throat was swabbed multiple times to test for infections and in the meantime I was put on a round of steroids to bring down the swelling.
January 29: My infection tests came back negative and my PCP stated that it was important for us to do an ultrasound next.
February 1: Ultrasound appointment - check!
February 9: The ultrasound showed that I had multiple swollen and calcified lymph nodes, which explained why the lymph nodes on my neck felt like hard marbles under my skin. My PCP referred me to an ENT doctor and I called to make an appointment. The first available was February 13. When I confirmed my birth date with the scheduler, she said, “Oh that’s not a very fun way to spend a birthday.”
February 13: Happy 33rd birthday to me. My present? An endoscopy. That’s a short procedure where a provider takes an endoscope (a flexible tube with a light and camera attached to it) and sticks it through your nose and down your throat to get a better look inside. My ENT doctor confirmed that I have a deviated septum and that, while he wasn’t “too concerned,” our next steps were a CT scan and fine needle aspiration biopsy. We needed clearer imaging and we needed an actual sample of my lymph node.
February 22: CT scan appointment - check!
March 6: For my FNA biopsy, my appointment was at UCHealth Anschutz, the hospital where Aaron works. While getting transported to the operating room I saw signs up above for different ICUs and it dawned on me that a couple of floors above was where Aaron spends his days in the Surgical Trauma ICU. During my biopsy, they used local anesthesia to numb the area and inserted a long needle into the node I’ve since referred to as “the mothership” aka the angriest and most swollen node toward the front of my neck. My doctor inserted the needle once. Checked with pathology. “We need more tissue.” Second poke. Patho check. “We need more tissue.” This happened two more times, for a total of four rounds of this yanking and pinching before I was off the hook.
March 8: My FNA biopsy results hit my online health portal. I read “Negative for significant phenotypic abnormality. Negative for abnormal B-cell or T-cell population.” I thought to myself, Negative blah blah blah — that seems promising, right? Only in hindsight do I realize now that I missed the note further down in the report that said, “Please correlate with concurrent cytopathology report.” I thought I was in the clear and had mentioned this “good news” to Aaron, my parents, and a few of our friends.
March 14: It was one of our best snow days of the year and it was marvelous. In the evening, I saw an email notifying me that I had a new test result in my online health portal. When I opened it, I read “Compatible with Hodgkin’s Lymphoma.” I asked Aaron to come read it. We cried, we Googled to get our bearings on what this might mean, and most importantly, we prayed, and made plans to call my ENT doctor the next morning to understand if I had an official diagnosis.
March 15: At lunchtime, we did what we often do when we need a moment of calm: We get breakfast biscuits from Rise & Shine and head to Wash Park for the sunshine. The snow from the day before was thick and sparkling, already transfigured into a dozen snowmen blobs that we passed by on our way to the dock where Aaron proposed exactly four years prior. We felt overwhelming peace in our circumstances and I knew God was near to us as we sought to find our footing in this familiar place together. After spending all day in surgery, my ENT doctor was kind enough to call me that evening so that I didn’t head into the weekend wondering. He confirmed that the testing was conclusive, that I had “Classic Hodgkin’s Lymphoma,” and that he would follow up on Monday with next steps.
March 18: While at the gym, my ENT doctor called and told me that we needed more tissue to determine pathology. He’d like to move quickly and do an excisional biopsy of a lymph node and, Can I be available for surgery the next day? You bet. No food/water after midnight and no lifting or climbing for two weeks after. Shoot. I decided in that moment to turn my upper body workout into a full body workout and you best believe I soaked in every last sweet rep before heading home.
March 19: On the day of surgery, my ENT doctor was energetic, kind, fast-talking, and confident — just the type of guy you want slicing into your neck. :) The mothership node was taken down and I went home with Jello and a cheese stick, all while talking absolute nonsense to Aaron as I returned from anesthesia dreamland.
March 22: Chemotherapy and radiation can damage fertility so Aaron and I were connected with a fertility clinic to discuss my options as an oncology patient. After an ultrasound, blood draw, and a bunch of tests, we met with two doctors to review my numbers. They explained the process and commitment of egg retrieval and freezing and what future embryo creation and IVF would involve — all things that Aaron and I were pretty unfamiliar with before this. We asked a lot of questions and expressed a lot of concerns, and ultimately left with much to consider.
March 26: The day we met my oncologist! He provided an overview of Hodgkin’s Lymphoma, ordered a bunch of diagnostic tests, and discussed treatment options with us.
Week of April 1: A big appointment week. I completed my echocardiogram and pulmonary function tests which were used to check that my heart and lungs were in a healthy place ahead of chemo. I also had my first-ever PET scan. For this full-body scan they inject a radioactive sugar tracer into your blood after a period of fasting, pass you slowly through a giant scanner for about 30 minutes, and the parts that light up help illuminate areas where cancer cells are present.
April 8: We met with the NP on my team to review staging results and I was officially diagnosed with “Classical Hodgkins Lymphoma Stage 2a early favorable” — which was exactly the news we were hoping and praying for! My PET scan showed that the cancer was present in my neck and chest, but had not spread below my diaphragm, or into organs or bone marrow. We also completed a “chemo teach” session where we went over the chemotherapy process and side effect management in much greater detail.
April 11: I had surgery to implant my chemo port which will remain in place for the duration of chemotherapy. My surgeon shared that he was a Hodgkin’s Lymphoma survivor, which was an encouragement to us! He showed me his port scar and said, “I really do know how this feels.”
A port is a small device placed under the skin on my chest and the catheter connected to it is inserted into the superior vena cava vein that feeds into my heart. This allows chemo drugs to be administered directly to a large vein and benefits include reduced risk of vein and tissue damage, less infection risk, and no more need for IVs since the port will be used for all of my future blood draws and chemo treatments. I made a comment to Aaron and referred to it as my “Voldeport” and he goes, “Ohhhhh, because you’re going to be bald, right?” LOLLL. Well, yes and no. I just thought it seemed like an apt name for this foreign horcrux in my chest — it has its benefits for now, but one day I’ll be glad to be free of it.